Causes of exocrine pancreatic insufficiency ( EPI)
Diabetes, chronic pancreatitis, cystic fibrosis, and more
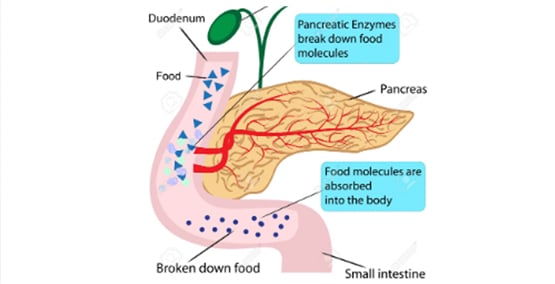
-Exocrine Pancreatic Insufficiency (EPI) usually results from a disease or condition that affects the pancreas, an injury or surgery in the area.
The most common causes of EPI are:
Rarely EPI causes:
- Shwachman-Diamond syndrome
- Cancer
- Zollinger-Ellison Syndrome
- Johansson-Blizzard Syndrome
- the need for surgery on the pancreas
The Conditions
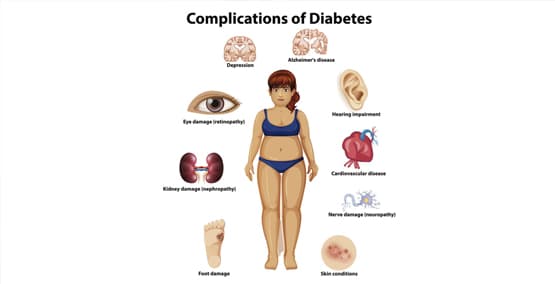
Diabetes causes EPI in as many as 75 percent of people who need insulin (mostly Type 1 diabetes) and 50 percent of people who have Type 2 diabetes. It is especially common in people who have had diabetes for a long time, who need high doses of insulin and who have trouble cpntrolling blood sugars.
There are lots of causes of chronic pancreatitis with all of them resulting in damage to the cells in the pancreas that make digestive enzymes, leading to EPI. Chronic pancreatitis can also damage the cells that make insulin, causing diabetes. When chronic pancreatitis causes both diabetes and EPI, this is sometimes called Diabetes type 3.
In cystic fibrosis, the body makes thick mucus that blocks the channels in the lungs, digestive system and other organs. The mucus blocks the channels in the pancreas that transport digestive enzymes from the pancreas to the digestive tract, leading to EPI. About 90 percent of people with cystic fibrosis develop EPI.
Schwachman-Diamond Syndrome is a rare condition that affects the pancreas, bone marrow, and bones. It is inherited genetic disorder. EPI typically shows up in early childhood. But about half outgrow their EPI as they get older.
Pancreatic cancer and surgery to treat the cancer can lead to EPI. This is extremely rare in children. The cancer cells replace the cells that produce digestive enzymes and the tumor may also block enzymes from entering the digestive tract.
Surgeries where a large part of the pancreas is removed or where the channel that connects the pancreas to the intestine (the pancreatic duct) is removed can also result in EPI.
Zollinger-Ellison Syndrome is another rare condition producing large amounts of stomach acid. The stomach acid can stop pancreatic enzymes from working, causing EPI. Other acid conditions can also interfere with digestion so an acid blocker is usually prescribed.
Rare cases of EPI can occur with celiac disease, but treatment with a gluten-free diet usually takes care of the EPI.
Inflammatory bowel disease (IBD) with either Crohn's disease or ulcerative colitis can be associated with EPI when the medicines used to treat IBD cause pancreatitis. The pancreatitis seems to be what causes the EPI, not the IBD.
Patients who have had gastric bypass surgery can look like they have EPI, because they often share the same symptoms of decreased absorption, gas, bloating, and fullness after eating small amounts. But they do not have EPI.