Diabetes in cystic fibrosis
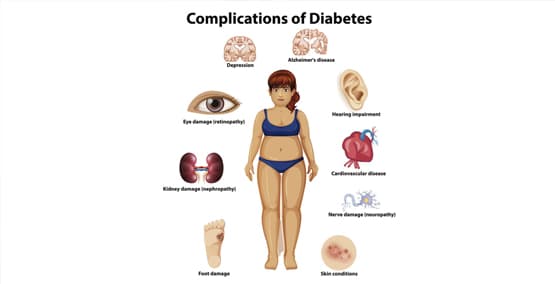
Cystic fibrosis (CF) is the most common cause of exocrine pancreatic insufficiency (EPI) but it has also been associated with both Type 1 and 2 diabetes. Why? Because the endocrine cells of the pancreas also affect the cells that produce insulin.

As many as 25% of those with CF will develop diabetes by 20 years of age and 35-40% will eventually develop diabetes. The diabetes is usually a milder form, and many will have also have unexplained weight loss.
Cystic fibrosis (CF) is a disease that affects the lungs, pancreas, intestines and reproductive tract. The cells in the pancreas that cystic fibrosis affects are called the exocrine cells which also make the enzymes that help the body breakdown the foods we eat. When the exocrine pancreas does not work (EPI) that causes poor weight gain and oily, foul-smelling stools due to fat malabsorption. Often, certain nutrients and fat-soluble vitamins A, D, E, K, are poorly absorbed and lacking in the body.
Those with diabetes can also develop EPI
As many as 50% of those with Type 1 diabetes and 33% with Type 2 diabetes can develop EPI. Their endocrine cells aren't producing insulin and their other cells don't produce the digestive enzymes they need either. They don't have cystic fibrosis, rather it is EPI. The EPI can be difficult to detect because there are not the classical symptoms of diarrhea, abdominal pain, foul smelling stools or flatulence (gas). EPI can be diagnosed with the correct tests.