Diagnosing pancreatic insufficiency (EPI)
The questions, tests, and treatments for EPI
-Exocrine Pancreatic Insufficiency (or EPI) isn't always easy to recognize. A thorough medical history of your problems or your child's is needed to learn about your eating habits.
How quickly do you get full? Do you have gas and bloating? Do certain foods make the pain and discomfort worse? Your doctor will ask these questions and more about your bowel movements and whether anyone else in the family has similar problems.
A physical examination will check your abdomen and skin for any signs of a vitamin deficiency.
Information gathered from the history and physical examination is then used to direct further testing.
Causes of pancreatic insufficiency
In children, the cause can be from a genetic defect like cystic fibrosis, a condition called Schwachman-Diamond Syndrome or a problem with the structure of the pancreas.
These pancreatic conditions carry over into adulthood.
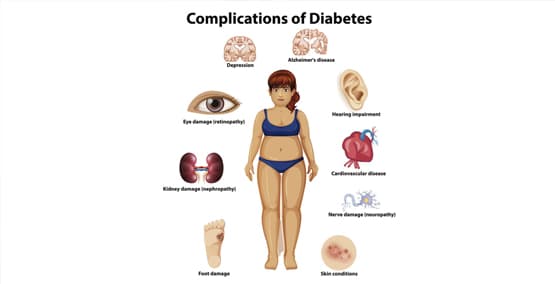
Patients with diabetes can also develop pancreatic insufficiency over time as can people who have had abdominal surgery or repeated bouts of pancreatitis.
Symptoms of pancreatic insufficiency
When the enzymes are not working fully, the body isn't able to digest and absorb nutrients. Fats tend to be the most affected which can lead to weight loss or difficulty gaining weight.
Unabsorbed nutrients go down into and through the intestine, often causing bloating, gas, discomfort and oily diarrhea. Because fats also are important in absorbing fat soluble vitamins A, D, E, and K, patients can also develop vitamin deficiencies, causing vision problems, bone pain and anemia.
Not surprisingly, almost half of those with ongoing gastrointestinal (GI) complaints wait to see if their symptoms get better before going to a health care professional. Sometimes adults wait an average of over 3 ½ years to seek that help, according to a Harris Poll**. Sixty percent of patients said the delay was because they were embarrassed of their symptoms. That survey also indicated that 45 percent of the 1001 patients contacted were unsure of the role the pancreas in digestion and only 22 percent were aware of the symptoms of EPI.
It's important not to wait to talk to your doctor if you have any of the following sypmptoms:
- Bloating
- Gas
- Abdominal Pain or Discomfort
- Diarrhea
- Oily film in the toilet
- Weight loss
- Vision problems
- Bone pain or breaks
- Anemia
Laboratory testing
The three main tests used to diagnose EPI are the fecal fat, fecal elastase and pancreatic stimulation.
Fecal fat test measures the amount of fat in the stool. It can be used to look for greasy stools in a single specimen. A 3-day collection can determine how much fat the body is wasting. A high amount of fecal fat indicates a problem with absorbing fat. The test also helps to show if treatment with enzyme replacement therapy (PERT) is adequate or if more is needed. Further testing may be required to determine the cause.
Fecal elastase test measures the amount of this enzyme in a bowel movement (often at the same time a fecal fat is tested). Elastase is produced by the pancreas to help breakdown protein. A deficiency of elastase is an indicator of EPI.
Direct pancreatic function test, also called pancreatic stimulation test, measures how much enzyme the pancreas produces. A medicine that mimics the natural hormones produced by the body is given and then samples are taken. This test is usually performed only at specialized centers because it requires sedation and endoscopy.
Tests for narrowed ducts
Two procedures are available to view the pancreatic ducts that drain the pancreas if there is concern that they may be blocked or misshapen. An MRCP (magnetic resonance cholangiopancreatograph) is a x-ray-like procedure that can show what the ducts. If there is a blockage, an ERCP, an endoscopy can be used to remove stones or open a narrow duct.
Treatment
Exocrine Pancreatic Insufficiency (EPI) is usually treated by replacing the enzymes that aren't present or functioning fully. Because the enzymes need an alkaline environment to work, sometimes an acid blocker is also needed.
** Conducted on behalf of the American Gastrointestinal Association, reported in Jan 2017 in GI and Hepatology News.