
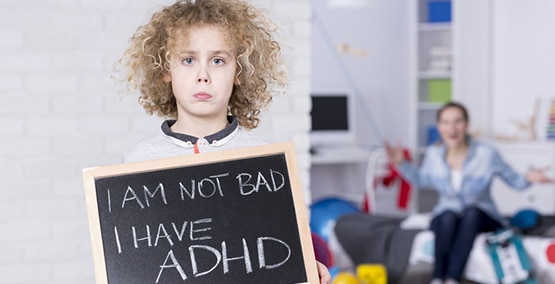
How to get kids with ADD and ADHD to eat
It can be hard to get kids with ADD or ADHD to eat. Mealtime can be frustrating because of their lack of focus (or their focusing on the smallest details), so they often want to get up from the table or play instead of eat. It's often more taxing to take them to a restaurant, with the different decor and a hundred new things ready to grab their attention.
Even on one of those wondrous medications that help them focus and perform previously impossible school tasks, eating is a challenge, and maybe more of one, because the main side effect is a loss of appetite. Many kids need the medicines even on weekends and vacations. As a result, some have difficulty gaining weight.
Here's what you can do to help them eat, gain and grow.
Choose healthy foods for meals and snacks. Avoid letting them snack on chips, cookies and crackers. They don't need those extra carbs, even though they are a big source of calories. Instead, have carrot sticks and other crisp veggies that they can dip in hummus or yogurt, fruit or bite size meats and cheese ready for after school snacks. They'll get their calories, but plenty of protein and other micronutrients. If they are on ADHD meds, add a sandwich or small entree (a loaded baked potato or a few chicken tenders) after school–then have dinner 2 to 3 hours later, so they'll be hungry again.
Don't offer drinks until the end of meals. Too often kids fill up on less nutritional fluids at the beginning of a meal and then they don't want to eat what's on their plate.
Start with a good breakfast. The Sunday Special I call it, eggs, whole grain toast, fruit and maybe a meat if they have time; or oatmeal or other high fiber cereal topped with fruit and either yogurt or milk. sounds great, except many kids are rushing out of the house. In that case, try a powerhouse breakfast smoothie: two fistfuls of fruit (fresh or frozen), 1 fistful of spinach (the fruit masks the taste), a packet of instant breakfast or a weight gain powder from a sports or nutrition store) and then juice or yogurt for taste and to make it liquid, so they can drink it easily.
Don't expect them to eat lunch at school, especially if they are on medication. Send along some cheese, celery sticks with peanut butter, or something else to tempt them to eat. Bailey Koch, on our advisory board, finds that some kids do well with a protein bar and a glass of milk. And some will prefer one of the "complete" nutritional drinks, like Boost or Pediasure.
Make dinner their major, well-balanced meal. Hopefully, the medicine will wear off by then. But make sure they come to the table hungry, so no snacks and nothing to drink for at least an hour or so beforehand. And don't trip over your efforts by having a drink on the table. An ounce or two perhaps, but save the rest for the last part of the meal.
End the evening with what my patient's call Dr. Cohen's Super Shake. It's the same principle as the morning smoothie. A tasty milk shake with instant breakfast or the same weight gain powder added in. For those who are lactose intolerant or milk allergic, substitute soy or rice products or the AM smoothie. This is not recommended for those with reflux, sleep problems or asthma. It could make those conditions worse. and it shouldn't be pressed into the schedule if there's little time between dinner and bedtime–but maybe it could be used on weekends.
Turn off distractions during meals. TV, cellphones, tablets, video games. Try to get a conversation going to help teach good mealtime behaviors and to keep them at the table longer so they'll perhaps eat a little more.
Don't force feed. In other words, let them feed themselves, even if you have to cut the food into smaller pieces. Too many negative psychological implications if you are still spoon feeding or playing the games you did when they were toddlers.
At restaurants, make sure the kids go there hungry. Again, hold snacks before you get there. And resist the waiter's offer to bring something to drink at the start. Do try to understand their tolerance and frustration, sitting there while you finish your meal and pay for it. Consider your goals for the meal and your own patience with them as they grow impatient with the sitting. A handy toy or video game or simply crayons and paper may absorb them while they're waiting for their meal and afterward (but not during the meal).
Monitor your progress. Do a calorie count or use our food diary if you are really curious. Also, watch their weight. We would like to see usually a half-pound a month before puberty and whatever catch-up gain is needed; after puberty, set the goal with a dietitian or your doctor). Also make sure the urine is plentiful and light colored. If it's darker, more fluid should be added.




